4.30.2024 | by Vernon R Stanley, MD, PhD | ECGcourse.com | All rights reserved.
Welcome to this ECG Rhythm Quiz & discussion. Learning to read an ECG Rhythm strip, from the vantage point of Lead II can be a daunting task. In this blog, we roll our discussion back to the basics. Let us review some basics of ECG Rhythm analysis.
Enjoy this free printable to share with colleagues and students.
Quiz: Please analyze the following 3 ECG rhythm strips and select your answer from options below each strip. Answers are discussed within the blog and also at end of post.
Question 1
- Atrial Flutter
- Sinus Tachycardia
- Supraventricular Tachycardia (SVT)
Question 2
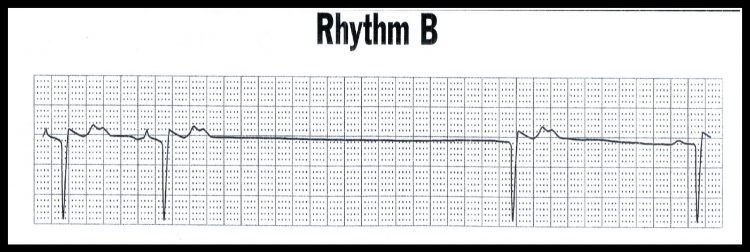
- Bradycardia
- Asystole
- Sinus Arrest with Junctional Escape Beat
Question 3
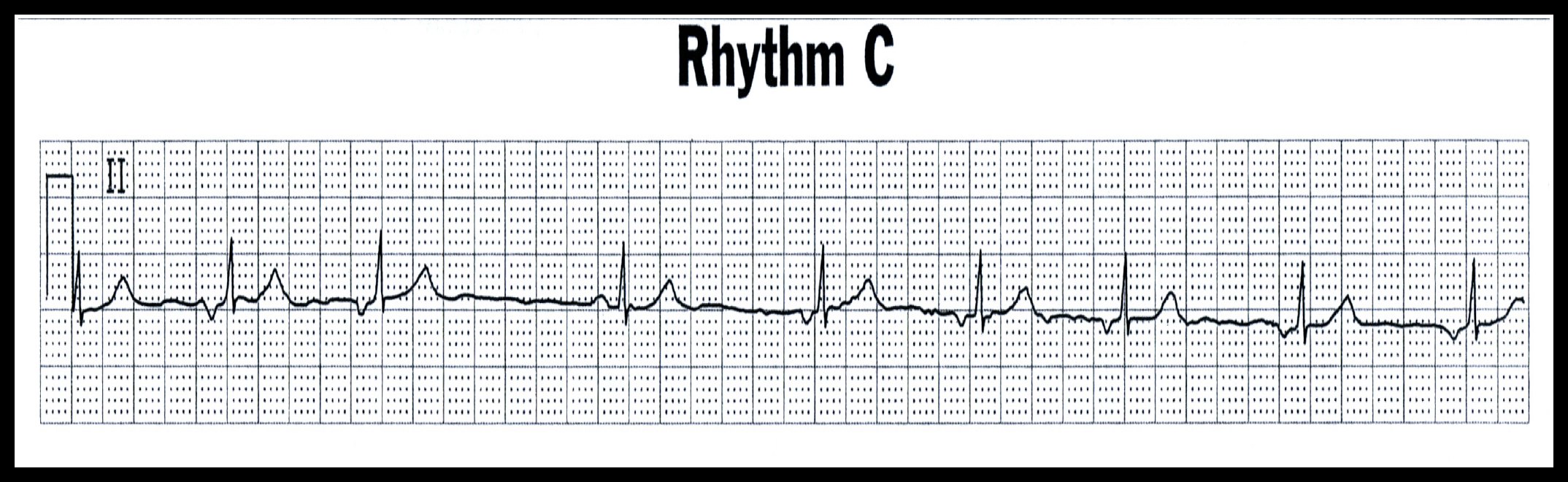
- Junctional Rhythm
- 2nd Degree AV Block Mobitz II
- Sinus Dysrhythmia
We will now begin this discussion with a review 6 of the more commonly encountered ECG Rhythms in medicine.
- Normal Sinus Rhythm
- Sinus Tachycardia
- Sinus Arrest with Junctional Escape Beat
- Junctional Rhythm
- Atrial Flutter
- Supraventricular Tachycardia (SVT)
Please note, the above 6 rhythms are not meant to be, in any way, a complete discussion of all the ECG Rhythms you will need to know. These are simply 6 examples of the more common ECG Rhythms you will encounter in your everyday practice of medicine. For a more thorough discussion of ECG Rhythms from ECGcourse.com, please see the Animated Rhythms Course. To recertify or find an in-person class, check out ACLS and PALS Training.
Below is a sample taken from the Animated Rhythms Course of a Normal Sinus Rhythm animated tutorial (please note the full content is only available to paid subscribers).
Propagation of the electrical signal of the ECG Rhythm
Before discussing recognition of the different ECG Rhythms, it is important to correlate the anatomical region where the electrical signal is generated with the electrical signal generated on the ECG rhythm strip. In a normal, healthy heart, the electrical signal initiates in the SA (sinoatrial) node, depolarizes the Atrial myocardium, depolarizes the AV (atrioventricular) node, propagates through the Bundle of HIS, and terminates in the Purkinje cells, depolarizes the Ventricular Myocardium (endocardium to the epicardium). The myocardial tissues then recharge (repolarize) and the SA node discharges again; the cycle then repeats itself.
Where:
- 1 = time at depolarization of SA node
- 2 = time at depolarization of AV node
The resultant electrical signal on the ECG Rhythm is as follows:
- P = Depolarization of the Atria
- QRS = Depolarization of the Ventricles
- T = Repolarization of the Ventricles
Important Note: The depolarization of the SA node (at 1) and the AV node (at 2) produce only a tiny voltage and will not be visible on the standard rhythm strip.
Electrical characteristics of myocardial (heart) tissues
It is essential that you understand the electrical characteristics of the heart tissues. This will aid you in understanding the normal ECG rhythm characteristics as well as the common ECG dysrhythmias that you will encounter in your practice.
The heart is composed of two basic tissue types:
- Tissue #1. The myocardium (muscle).
- Tissue #2. The special electrical conduction system*.
Electrically speaking, the two tissue types are characterized as follows below:
Tissue 1. The myocardium does not possess automaticity and subsequently will not depolarize until stimulated by an external stimulus. This stimulus is usually the adjacent Purkinje Cell or an adjacent myocardial cell in the active process of depolarizing.
Tissue 2. The special electrical conduction system has two important unique properties:
- a) It possesses automaticity, i.e., it will spontaneously depolarize and repolarize without an external
stimulus. - b) It conducts the electrical signal very rapidly as compared to other tissues.
Tissues with Automaticity include:
- SA Node, aka SinoAtrial Node (60-100 bpm)
- Internodal Pathway (Atria; 60-80 bpm)
- AV Junction Node (40-60 bpm)
- Bundle of HIS (& all branches; 40-60 bpm)
- Purkinje Cells (20-40 bpm)
Important properties of Automaticity Tissues:
The automaticity tissue of the heart is designed to provide an automatic electrical stimulus to ultimately depolarize the myocardial tissue. The system is designed with a built-in demand backup as its fail-safe mechanism. The design function is as follows:
- If normal Sino-Atrial Node function…
SA Node discharges at a rate of 60-100 bpm. This signal will suppress all the other automaticity tissues. - If the SA Node fails…
The next in line automaticity tissue takes over as follows:
Atrial Internodal Pathways- discharge rate 60 – 80 bpm. (This signal will suppress all the lower hierarchy automaticity tissues.) - If the Atrial Tissue fails…
The next in line automaticity tissue takes over as follows:
Junctional (including Bundle of HIS and branches) – discharge rate 40-60 bpm. (This signal will suppress all the lower hierarchy automaticity tissues) - If the Junctional Tissue fails…
The next in line automaticity tissue takes over as follows:
Terminal Purkinje Fibers – discharge rate 20-40 bpm. - If the Purkinje Fibers fail…
Ventricle myocardium will receive no electrical signal. Flatline will follow, then death.
Now to review the following ECG rhythms strips (in order from “A” through “E”).
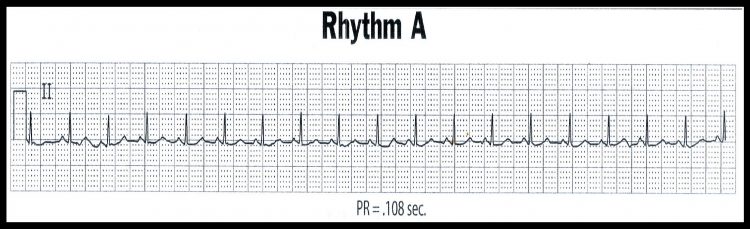
ECG Rhythm “A”
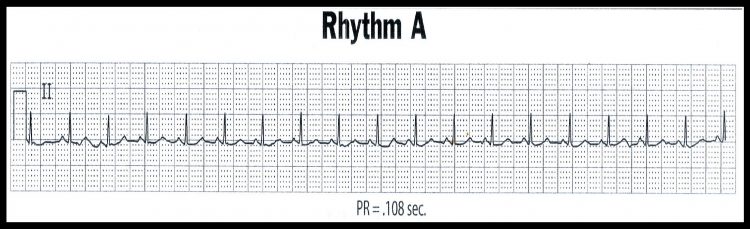
This is a benign rhythm and usually requires no treatment (unless hemodynamically indicated or patient is symptomatic).
The signal travels in a normal pathway from the SA node to the AV node to the Purkinje Cells, then across the
myocardium. The rhythm strips will appear normal except that the rate is rapid.
P-P interval = constant • QRS-QRS interval = constant
Characterized by:
- Rate > 100 beats per minute
- Otherwise all other parameters are normal.
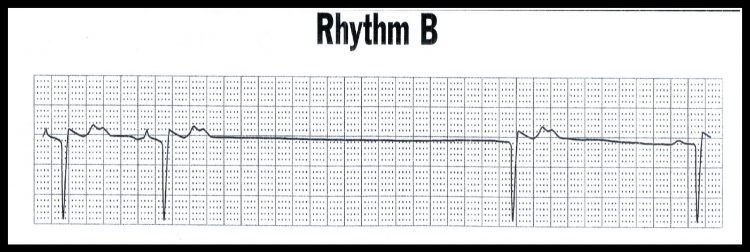
ECG Rhythm “B”
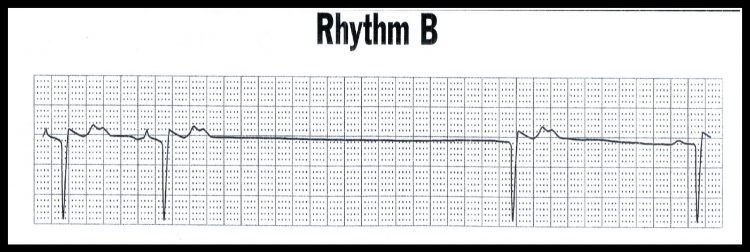
Sinus Arrest with Junctional Escape Beat
These are usually benign beats and most often require no emergency treatment unless a patient is symptomatic or is hemodynamically unstable.
Occurs after long hesitation (pause). Spontaneous discharge of automaticity tissue from:
Atrium ……………… Atrial Escape Beat
AV-Junction ……… Junctional Escape Beat
Ventricle …………… Ventricular Escape Beat
Common Error
An ectopic beat originating from the ventricle (because of its wide, bizarre shape) is sometimes referred to as a PVC (Premature Ventricular Contraction), even if the beat does not occur early. This is obviously incorrect. Conclusion: If the beat occurs later than expected, it is not a premature beat, but an escape beat.
Escape Beat characterized by:
- Spontaneous beats which occur after long pause of electrical activity.
- Named according to origin of beat: Atrial, Junctional or Ventricular
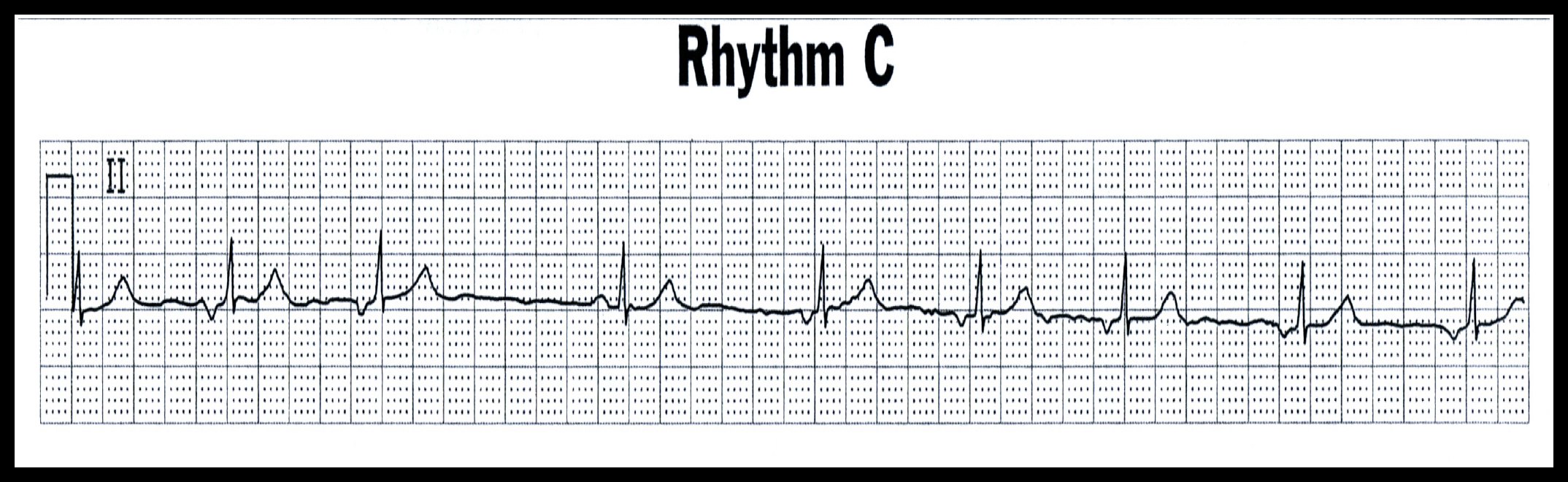
ECG Rhythm “C”
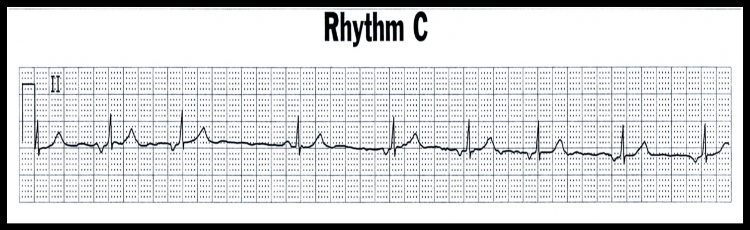
This is a benign ECG rhythm and usually requires no treatment (unless hemodynamically unstable).
There are 4 possible scenarios of the P-wave presentation
- P-wave precedes QRS complex
- P-wave coincident with QRS complex
- P-wave follows QRS complex
- P-wave is absent (is isoelectric)
The electrical signal initiates at junction, travels retrograde in the Atrium (therefore P-wave inverted); then it travels in a normal pathway direction (antegrade) through Ventricles –> the QRS complex is therefore normal appearing.
Junctional Rhythm characterized by:
- Inverted or sometimes absent P-waves
- Normal QRS complexes
- Regular rhythm
- Rate 40-60
ECG Rhythm “D”
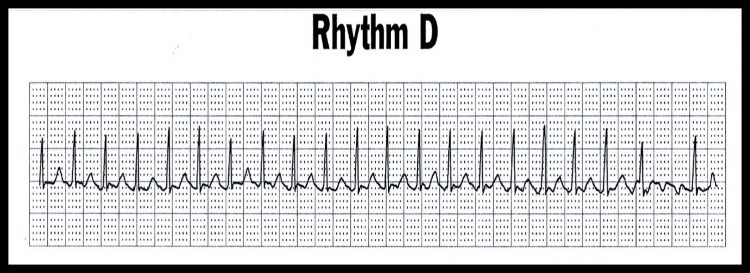
Atrial Flutter 2:1 (Ventricular Rate = 160)
The malfunctioning area of the Atria discharges at a rapid rate (commonly 300 beats per minute) and takes on a “sawtooth” pattern. Some of the flutter signals (f-waves) will be blocked at the AV node. You must therefore address this when describing the rhythm, e.g., Atrial Flutter with 2:1 Block, 3:1 Block or Variable Block.
Pearl regarding the Atrial Flutter rhythm: If ventricular rate of a cardiogram is 150 beats per minute, consider Atrial Flutter with 2:1 block. Please note, you may look at the entire 12-Lead ECG, and the flutter pattern may only be apparent in one or two leads.
Atrial Flutter is generally a more serious finding and sometimes requires more aggressive treatment. However, you must be diligent and correlate clinically, including comparison with the old ECG. The ECG Rhythm pattern might be chronic for this patient and the treatment may be none.
Atrial Flutter Characterized by:
- Atrial flutter waves (sawtooth pattern)
- Rhythm might be regular or irregular depending on block
ECG Rhythm “E”
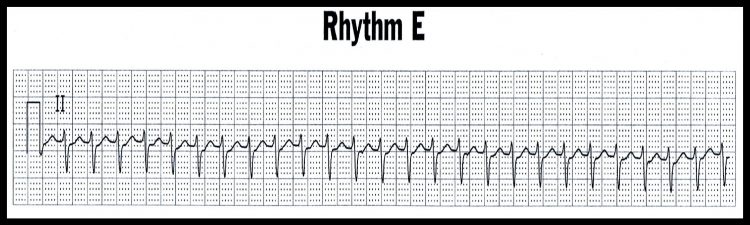
Supraventricular Tachycardia (SVT); Rate = 160 bpm
There is a spontaneous focus of irritability of the Atrium (supraventricular) that discharges at a rapid rate. [Please note that the term SVT is typically reserved for regular rhythms, either atrial (with p-wave often hidden) or junctional].
Pearl regarding the SVT: Often the P-waves of SVT (Supraventricular Tachycardia) cannot be discerned and sometimes may appear as a tiny notch. This is because the rate is so rapid that it blends with the T-wave.
If clinically indicated, treatment consists of vagal maneuvers and IV adenosine.
SVT is characterized by:
- Rate = 150-250 bpm
- Rhythm = Regular
- QRS complexes are narrow (unless a conduction defect of LBBB, RBBB or IVCD is present)
If you enjoyed this quick ECG Rhythm review, we invite you to take the Animated Rhythms Course (6 hours Cat I CME). The Animated Rhythms is our deluxe, hybrid online and book learning format which carries 6 hours of Category I CME or Nursing CE.
For a faster, “crash-course” study, you may want to check out the ACLS Prep Course (3 hrs Cat I CME/CE). This is online-only version of the Animated Rhythms and a very basic, simple, quick brush up on ECG Rhythms.
Both courses provide video animated tutorials with supplemental audio tools to help learn 26 of the most commonly encountered ECG rhythms in the practice of medicine.
ANSWER Key: Question 1
- Atrial Flutter
- Sinus Tachycardia
- Supraventricular Tachycardia (SVT)
ANSWER Question 2
- Bradycardia
- Asystole
- Sinus Arrest with Junctional Escape Beat
ANSWER Question 3
- Junctional Rhythm
- 2nd Degree AV Block Mobitz II
- Sinus Dysrhythmia
-
Advanced 12-Lead ECG Interpretation Course (30 Hrs CME)
$499.00 -
50 ECG Case Studies Course (13 Hrs CME)
$145.00 -
Animated ECG Rhythm Interpretation Course (9 Hrs CME/CE)
$125.00 -
STEMI Recognition Review Course (6 Hrs CME)
$90.00 -
Intensive ECG 3-course Suite: (49 Hrs Cat I CME/CE)
$769.00Original price was: $769.00.$699.00Current price is: $699.00. -
ECG Rhythms Field Guide Book
$48.50 -
Rhythm Ruler Pocket Guide
$14.50Original price was: $14.50.$9.95Current price is: $9.95. -
HEART Ruler Mnemonic Pocket Guide
$15.00Original price was: $15.00.$9.95Current price is: $9.95. -
ACLS Prep Course (3 Hrs CME)
$65.00